Clinical trial technology is supposed to streamline operations, not slow them down. But too often, the stack becomes the source of delay. This checklist outlines 7 must-haves in a true e-clinical platform so you can assess whether your systems are built to lead or are holding you back.
What may being as a smart best-of-breed approach can often evolve into operational complexity that compounds with every new study. With Electronic Data Capture (EDC) from one vendor, Clinical Trial Management System (CTMS) from another, and Electronic Trial Master File (eTMF) housed elsewhere, things get complex fast.
The assessment framework below is designed to help you evaluate your current environment across seven essential capabilities. It reveals whether your tools support the direction of modern clinical development or are anchored in outdated, disconnected approaches.
The True E-Clinical Platform Assessment
1. Native Integration Across Core Functions
- The Standard: Your EDC, CTMS, eTMF, Randomization and Trial Supply Management (RTSM), and Electronic Patient-Reported Outcomes (ePRO) systems should operate within a single platform architecture. If they require five separate logins and multiple middleware connectors, you are working against efficiency.
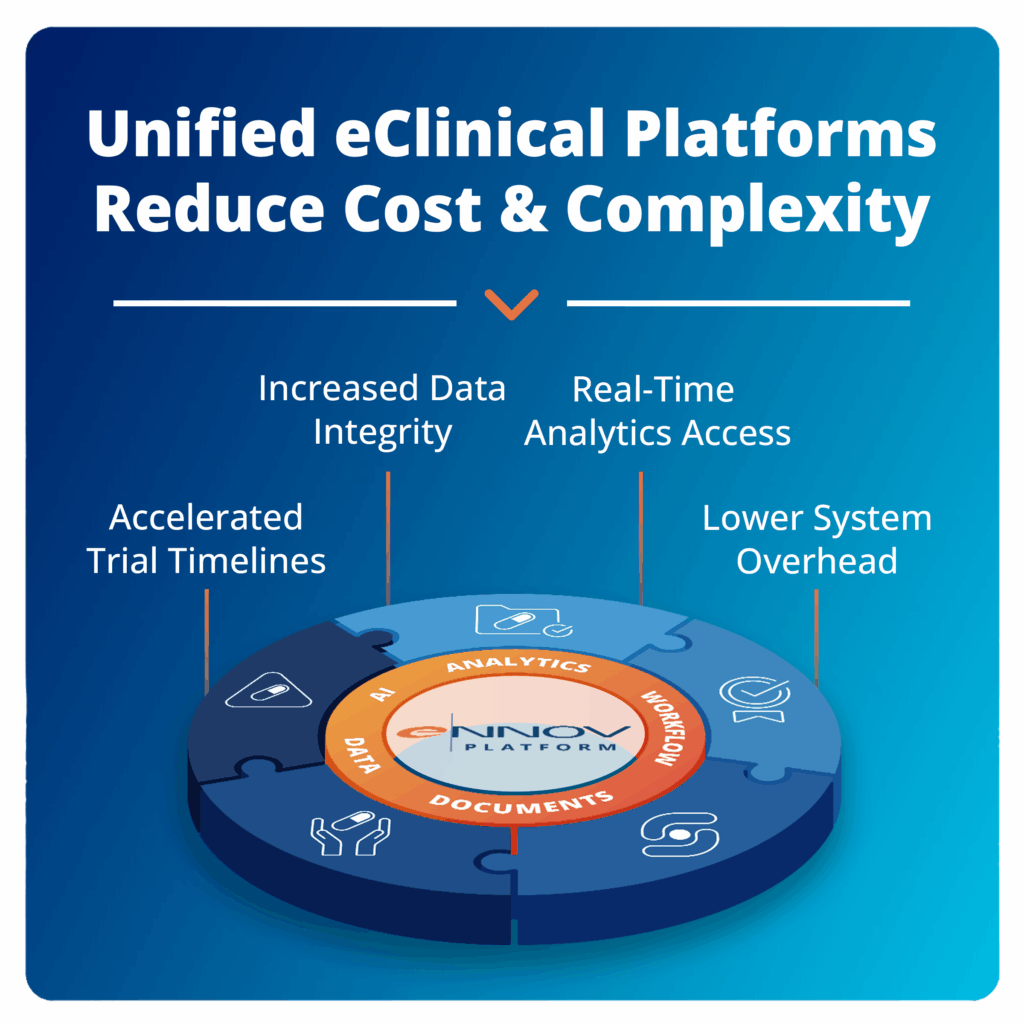
- Why It Matters: True E-Clinical platforms unify study conduct from startup through submission. Native integration eliminates data transfer delays, reduces validation overhead, and provides real-time visibility across all study functions. When systems are inherently connected, teams spend less time managing tools and more time managing trials.
- Assessment Question: Can your team access all core study functions through one login, with real-time, bidirectional data flow between modules?
2. Flexible, Mid, Study Change Support
- The Standard: Protocol modifications should not require full system rebuilds, extended downtime, or cascading validation exercises.
- Why It Matters: Protocols evolve as safety data emerges, regulatory input is received, or operational challenges arise. Modern platforms allow for protocol amendments, visit schedule updates, and form revisions through dynamic configuration rather than hard-coded changes. This flexibility reduces delays and helps maintain study momentum.
- Assessment Question: When protocol amendments occur, can your system apply changes within days instead of weeks, without disrupting data collection?
3. Risk, Based Oversight, Built In
- The Standard: Risk-based monitoring should be a native feature, not a third-party add-on or manual workaround.
- Why It Matters: ICH E6(R3) emphasizes proportional monitoring and digital oversight. Effective platforms provide built-in access controls, audit trails, and central dashboards to identify and manage risk proactively. These tools help you stay inspection, ready and enable better oversight across studies.
- Assessment Question: Does your platform automatically surface risk indicators and generate audit, ready documentation, or are you stitching that together with manual processes?
4. Real, Time, Unified Analytics
- The Standard: Cross-functional insights should be available instantly through integrated dashboards, not manually pulled from multiple tools.
- Why It Matters: Effective study management requires immediate access to data, enrollment, safety, data quality, and more. Built-in analytics keep you close to your data, enabling seamless drill-down from visualizations directly to source forms without switching systems. This proximity to data also enables advanced capabilities like mass query generation from analytics insights, transforming how teams identify and address data quality issues across studies.
- Assessment Question: Can your team seamlessly navigate from analytics visualizations to underlying source data and generate actionable queries without leaving the platform, or are you limited to static dashboards that require separate systems for follow-up?
5. Patient, Ready Digital Tools
- The Standard: eConsent, ePRO, and Bring Your Own Device (BYOD) capabilities should be built into your platform and designed to support real patients, not just tech-savvy users.
- Why It Matters: Digital tools directly impact patient engagement, retention, and data quality. Multilingual, device, agnostic, and intuitive interfaces ensure accessibility. When these tools are fully integrated, they reduce site burden and improve data flow.
- Assessment Question: Do your patient-facing tools work seamlessly with your core study systems, or do they create friction and additional site workload?
6. Proven Compliance Foundations
- The Standard: Your platform should be validated and aligned with current and emerging regulatory frameworks, including ICH E6(R3).
- Why It Matters: Compliance isn’t just about checking a box. As global regulations evolve, your platform should offer adaptable workflows, comprehensive audit trails, and validated support for proportional oversight and traceability. This foundation helps you scale with confidence across geographies and trial types.
- Assessment Question: Is your platform equipped to meet future compliance standards, or will it need costly customizations and retrofitting?
7. One Source of Truth
- The Standard: All study stakeholders should rely on the same, authoritative data source, without duplications, versioning conflicts, or reconciliation.
- Why It Matters: Data integrity is non-negotiable. When multiple systems hold different versions of the truth, you risk errors and delays. A unified platform ensures consistency, accelerates decisions, and builds trust across the trial.
- Assessment Question: Does your team know exactly where to find the latest data, or do they spend time verifying across systems?
Quick Assessment: Is Your System Unified?
If you answered “Yes” to most or all of these, your platform is ready for modern trial demands.
If not, it may be time to re-evaluate whether your tech stack is keeping pace with your goals, or standing in the way.
Unify Your Stack, Multiply Your Impact
Fragmented systems drain time, budget, and focus, especially as trials grow more complex and timelines compress. Managing vendors, syncing tools, and reconciling data only gets harder with scale.
Unified platforms shift that burden. Instead of managing technology, teams can focus on executing the trial.
That’s why platform consolidation is now a strategic imperative. As regulations evolve and pressure mounts, your infrastructure must accelerate development, not create drag.
Ennov is recognized as a Representative Vendor in the Market Guide for Life Science E-Clinical Systems. Our unified Clinical Suite addresses each of the seven must-haves through native integration, enabling speed, oversight, and future-ready compliance.
If your current platform is showing its limits, ask yourself: what could your team achieve with one system purpose, built for clinical excellence?
The Market Guide for Life Science E-Clinical Systems offers expert insight into this shift.
Ennov is offering complimentary access for a limited time. Get the Report.


